
Noriaki Emoto
Professor at the Department of Clinical Pharmaceutical Science, Kobe Pharmaceutical University; and Visiting Lecturer at the Division of Cardiovascular Medicine, Kobe University Graduate School of Medicine
Graduated from Kobe University School of Medicine, 1987. After clinical residency in the Department of Internal Medicine and Division of Cardiovascular Medicine, entered Kobe University Graduate School of Medicine in 1990. Overseas study at the University of Texas Southwestern Medical Center from 1991. Returned to Japan as a Research Assistant at the International Center for Medical Research (ICMR), Kobe University Graduate School of Medicine, in 1997. Lecturer at the Division of Cardiovascular Medicine, Kobe University Graduate School of Medicine, involved with medical practice and research, since 2000, appointed Professor, and in current post since 2008.
Clinical specialties: hypertension and pulmonary hypertension. Research theme: vascular biology. Aiming to contribute to translational research by means of both medical practice and experimental research.
Cardiovascular and cerebrovascular diseases such as myocardial and cerebral infarction are caused by atherosclerotic disease1. Atherosclerotic diseases are the cause of approximately 25% of deaths in Japan, and constitute a major threat to the Japanese population, so there is a very high societal demand for these diseases to be defeated.
Treatment of atherosclerosis has previously focused on controlling the risk factors for cardiovascular disease development, represented by hypertension, diabetes, dyslipidemia, etc. Various risk factors are in fact increasingly controllable with renin-angiotensin system inhibitors, statins, etc. However, taking into consideration the continuing increase in the prevalence of cardiovascular diseases, there is an urgent need to establish new treatment strategies.
The response-to-retention hypothesis has been put forward for the mechanisms of onset and progression of atherosclerosis, and has been given considerable attention2,3. Accumulation of low-density lipoprotein (LDL) cholesterol and other lipids in vascular walls is considered to be a starting point for onset of early-stage arteriosclerosis, and it has recently been suggested that the structures of chondroitin sulfate chains in the tunica intima are connected to that accumulation, with the length of the chains being particularly closely connected4.
The present authors have put forward the following hypothesis: “Accumulation of lipids can be reduced by modifying the lengths of chondroitin sulfate chains, enabling prevention of or recovery from atherosclerosis”. Studies have since been performed to test this hypothesis, and the results are summarized here.
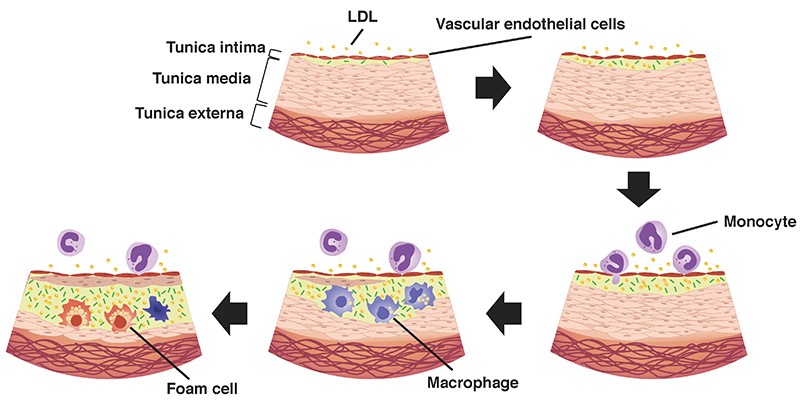
Blood vessels are composed of three layers; the tunica intima, tunica media, and tunica externa (Fig. 1). The tunica intima is in direct contact with the blood, and its surface is covered with a single layer of vascular endothelial cells. In addition to having a barrier function and anticoagulatory activities, the endothelial cells secrete various physiologically active substances, and support a range of physiological functions.
Atherosclerosis is a disease involving stenosis and occlusion of the arteries, caused by deposition of LDL in the arterial tunica intima, and atheroma formation by cells such as macrophages that have phagocytosed lipids (foam cells), smooth muscle cells that have invaded the tunica intima, and fibroblasts. It mainly develops in the large and medium-sized arteries, and is a cause of conditions such as acute myocardial infarction, cerebral infarction, and occlusive arteriosclerosis.
With respect to the mechanism of onset and progression of atherosclerosis, the response-to-retention hypothesis has been put forward for the initial stage of arteriosclerosis, and has been given considerable attention2,3. According to this hypothesis, firstly, lipids are deposited within the vascular walls (i.e. retention), the deposited lipids are then modified by oxidation, etc., forming oxidized LDL (ox-LDL), and macrophages respond to the ox-LDL by invading the tunica intima, with phagocytosis of lipids. It has been suggested that proteoglycans are involved in the deposition of lipids within the vascular wall4, but the details are unknown. The present authors have performed research relating to the hypothesis that the length of chondroitin sulfate chains in the tunica intima is linked to lipid deposition.
With respect to enzymes involved in chondroitin sulfate chain biosynthesis, numerous genes have been isolated and identified. However, among these enzymes, C4ST-1 and ChGn-2 have been shown to be particularly important for controlling chondroitin sulfate chain elongation6. In this respect, using LDL-receptor gene knockout mice, a murine arteriosclerosis model, arteriosclerosis was induced with a high-fat diet, and expression of each of the enzymes associated with arteriosclerosis progression, and progression of chondroitin sulfate chain elongation, were investigated. When mice of this model were given a high-fat diet, they developed arteriosclerotic lesions in 4 to 8 weeks. When chondroitin sulfate chain length was measured by gel filtration, it was shown that chondroitin sulfate chain elongation started during week 2 after initiation of the high-fat diet, and this was associated with progression of arteriosclerosis. Next, in order to confirm binding between lipids and chondroitin sulfate chains in the induced arteriosclerotic lesions, apolipoprotein B (apo B) staining was performed with samples treated with chondroitinase ABC (ChABC). Lipid-staining was found to be eliminated by ChABC, confirming binding between lipids and chondroitin sulfate chains. Together with progression of arteriosclerosis, increase in ChGn-2 and C4ST-1 expression was confirmed at the transcription level. On the other hand, no changes in ChGn-1 or C4ST-2 expression were found, suggesting that increases in ChGn-2 and C4ST-1 expression are involved in arteriosclerosis progression.
The above results suggest that in the arteriosclerosis disease model increases in ChGn-2 and C4ST-1 expression are associated with disease progression, and elongation of chondroitin sulfate chains in the tunica intima promotes lipid deposition.
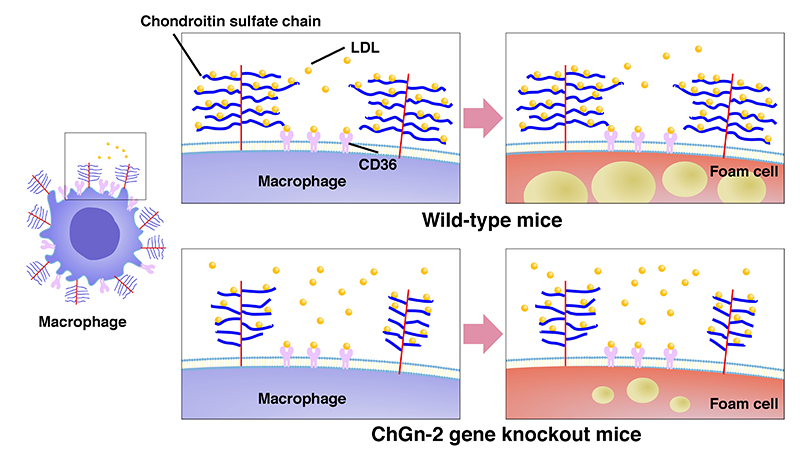
It is shown above that inhibition of ChGn-2 and C4ST-1 activity has potential as a novel therapeutic trategy for arteriosclerosis, mediated by inhibition of chondroitin sulfate chain elongation. In order to verify this possibility, the phenotypes of macrophages and foam cells, which are the principal structural elements of arteriosclerotic lesions, were investigated using ChGn-2 gene knockout mice.
Firstly, ChGn-2 knockout (ChGn-2-/-) mice were mated with LDL-receptor knockout (LDLR-/-), the offspring (ChGn-2-/-; LDLR-/- mice) were given a high-fat diet, and their arteriosclerotic lesions were analyzed. Progression of arteriosclerotic lesions in these dual-knockout (ChGn-2-/-; LDLR-/-) mice was significantly suppressed in comparison with the control group (ChGn-2+/+; LDLR-/-), although no differences between the groups were found in body weight, or in blood lipid indices such as total cholesterol and triglycerides. When the mechanism was analyzed, focusing on macrophages, it was shown that treatment of macrophages with lipids resulted in increased ChGn-2 expression, and chondroitin sulfate chain elongation. It was also shown that ChGn-2 promotes foaming of macrophages, and the mechanism for this was promotion by ChGn-2 of binding of lipids to macrophage surfaces, in addition to which it was shown that promotion of expression of a scavenger receptor, CD36, increased uptake of lipids (Fig. 2).
These results suggest that ChGn-2 increases the binding of lipids to macrophage cell surfaces, which is associated with progression of arteriosclerotic lesions due to promotion of foam cell formation.
Vascular smooth muscle is an important structural element of arteriosclerotic lesions. An important question is whether chondroitin sulfate chains in vascular smooth muscle have roles of some sort in progression of arteriosclerosis. As an approach to resolving this issue, carotid arteries were ligated into ChGn-2-/-; LDLR-/- mice to prepare a vascular intimal thickening model. In ChGn-2-/-; LDLR-/- mice, lipid deposition in the tunica intima was significantly lower than in the control group (ChGn-2+/+; LDLR-/-). In addition, the migratory activity of vascular smooth muscle cells isolated from the aortas of ChGn-2-/- mice was reduced by platelet-derived growth factor (PDGF). Furthermore, examination of the histopathological profile of the human coronary artery showed elevated expression of ChGn-2, which is consistent with arteriosclerotic lesions.
Taken together, it is suggested that ChGn-2 contributes to arteriosclerotic progression mediated by control of smooth muscle cell migratory activity, and that inhibition of ChGn-2 activity has the potential to inhibit progression of arteriosclerosis.
On the basis of the above study results, it can be suggested that ChGn-2 increases the uptake of lipids by macrophages as a result of chondroitin sulfate chain elongation in the tunica intima, and also that PDGF increases the migratory activity of vascular smooth muscle cells, resulting in progression of arteriosclerotic lesions.
In the unprecedented aging society that is approaching in Japan, it will be highly important to achieve healthy longevity, and it is therefore important to suppress arteriosclerotic diseases that reduce quality of life, such as cerebral apoplexy and myocardial infarction. The current series of research results suggests that vascular chondroitin sulfate chains, and ChGn-2, which adjusts the length of these chains, have potentials as diagnostic and therapeutic targets, with the aim of preventing onset and/or progression of arteriosclerosis. It is hoped that in future progress will be made with research aiming to establish treatments targeting chondroitin sulfate chains that can directly prevent and/or eliminate arteriosclerosis, irrespective of the presence or absence of diseases such as hypertension, diabetes and dyslipidemia.